Acute Renal Failure (ARF), also known as Acute Kidney Injury (AKI), is a serious medical condition characterized by the sudden loss of kidney function. This rapid decline disrupts the body’s ability to remove waste, balance electrolytes, and maintain fluid homeostasis, leading to potentially life-threatening complications. Understanding ARF involves delving into its causes, recognizing symptoms, and exploring treatment options, ensuring better awareness and management of this critical condition.
What is Acute Renal Failure?
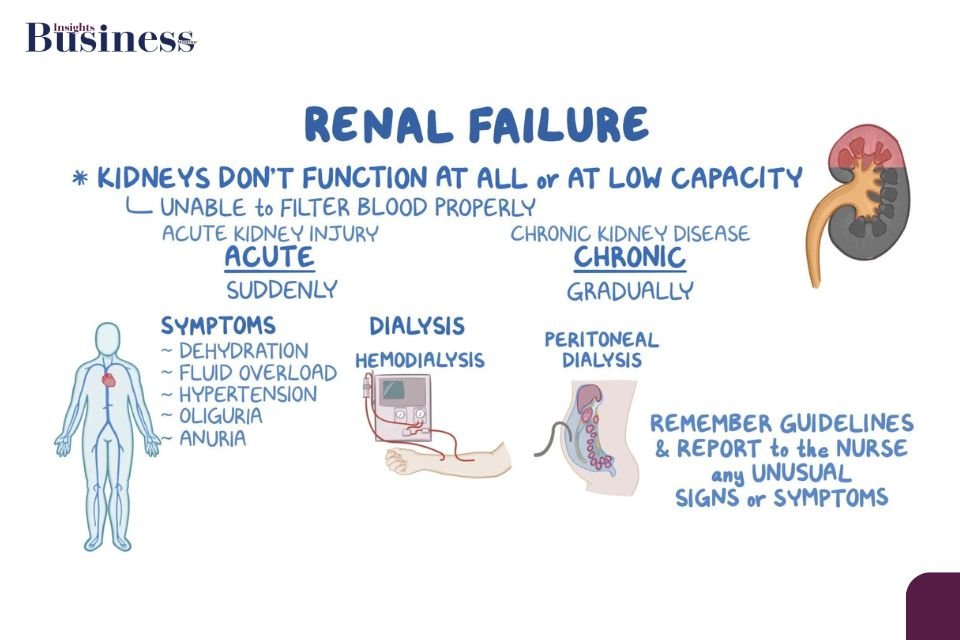
ARF is defined as a rapid and often reversible decline in kidney function, typically occurring over hours to days. Unlike chronic kidney disease, ARF is abrupt and may resolve with timely intervention.
- Key Functions of the Kidneys:
- Filtration of blood to remove toxins and waste products.
- Regulation of electrolytes and fluid balance.
- Production of essential hormones like erythropoietin.
When these processes are impaired, systemic complications arise, affecting overall health.
Causes of Acute Renal Failure
ARF is categorized into three primary types based on the location of the underlying problem:
- Prerenal Causes (Impaired blood flow to the kidneys):
- Hypovolemia (dehydration or significant blood loss).
- Low cardiac output (heart failure, myocardial infarction).
- Severe infections leading to septic shock.
- Liver cirrhosis causing hepatorenal syndrome.
- Intrinsic Causes (Direct damage to the kidneys):
- Acute tubular necrosis (ATN) due to toxins or ischemia.
- Glomerulonephritis or interstitial nephritis.
- Prolonged use of nephrotoxic medications (e.g., NSAIDs, antibiotics like aminoglycosides).
- Autoimmune conditions such as lupus nephritis.
- Postrenal Causes (Obstructions in urine outflow):
- Kidney stones.
- Enlarged prostate or prostatic hyperplasia.
- Tumors compressing the urinary tract.
Symptoms of Acute Renal Failure
Early detection is key to preventing complications. Common symptoms include:
- Fluid Imbalance: Swelling in the legs, ankles, or face due to fluid retention.
- Reduced Urine Output: Oliguria or complete anuria in severe cases.
- Electrolyte Disturbances:
- Hyperkalemia (elevated potassium levels causing arrhythmias).
- Metabolic acidosis (buildup of acid in the blood).
- Systemic Effects:
- Fatigue and weakness due to uremia.
- Nausea, vomiting, and loss of appetite.
- Altered mental status, confusion, or seizures in severe cases.
Diagnosis of Acute Renal Failure
- Clinical History and Physical Examination:
- Assessment of medical history, medication use, and recent illnesses.
- Identification of signs like edema, dehydration, or urinary abnormalities.
- Laboratory Investigations:
- Blood tests for creatinine, urea, and electrolyte levels.
- Urinalysis for signs of proteinuria, hematuria, or infection.
- Imaging Studies:
- Ultrasound to detect obstructions or structural abnormalities.
- CT scans or MRIs for detailed evaluation in complex cases.
- Biopsy:
- In select cases, kidney biopsy helps identify specific intrinsic causes.
Treatment Options for Acute Renal Failure
Managing ARF requires addressing the underlying cause and providing supportive care:
- Prerenal ARF:
- Restore blood flow with IV fluids or blood transfusions.
- Treat underlying causes such as heart failure or sepsis.
- Intrinsic ARF:
- Stop nephrotoxic medications immediately.
- Administer corticosteroids or immunosuppressants for autoimmune conditions.
- Initiate dialysis in cases of severe uremia or electrolyte imbalances.
- Postrenal ARF:
- Relieve obstructions using stents or surgical interventions.
- Catheterization for immediate relief in urinary retention cases.
Dialysis and Its Role in Acute Renal Failure
When conservative measures fail, dialysis is a life-saving intervention. Types of dialysis include:
- Hemodialysis: Blood is filtered through a machine to remove toxins and excess fluids.
- Peritoneal Dialysis: A catheter inserted into the abdomen allows for waste removal using a dialysis solution.
Prevention of Acute Renal Failure
Reducing the risk of ARF involves proactive measures:
- Hydration: Ensuring adequate fluid intake, especially during illnesses or heavy physical activity.
- Avoid Nephrotoxic Substances: Use medications responsibly and avoid excessive alcohol or illicit drug use.
- Manage Chronic Conditions: Control diabetes, hypertension, and heart diseases effectively.
- Regular Check-Ups: Monitor kidney function in high-risk individuals.
Complications of Acute Renal Failure
Untreated ARF can lead to severe complications:
- Chronic Kidney Disease (CKD): Prolonged ARF episodes can cause permanent kidney damage.
- Cardiovascular Issues: Fluid overload and electrolyte imbalances can strain the heart.
- Infections: Weakened immune response increases susceptibility.
Advancements in ARF Management
- Biomarkers for Early Detection:
- Innovations like NGAL (neutrophil gelatinase-associated lipocalin) enable quicker diagnosis.
- Regenerative Therapies:
- Stem cell research shows promise in repairing kidney damage.
- Precision Medicine:
- Tailored treatments based on genetic and molecular profiling are emerging.
Conclusion
Acute Renal Failure is a critical condition that necessitates prompt diagnosis and treatment. By understanding its causes, symptoms, and management, healthcare professionals and patients alike can mitigate risks and improve outcomes. As research advances, the future holds promise for even more effective strategies in combating this potentially reversible condition.